Introduction: Recently published data show that COVID-19 is characterized by a hypercoagulable ROTEM profile and decreased fibrinolysis. Multiple reports suggest that severe COVID-19 infection is associated with an increased thromboembolic risk. There are limited data associating a hypercoagulable ROTEM profile and outcomes in the literature. A hypercoagulable ROTEM profile could help identify patients at risk of worse outcome and help target a study population for enhanced anticoagulation therapy or other COVID-19 therapy.
Objectives: To determine if early hypercoagulability on ROTEM is associated with a higher risk of thromboembolic complications or worse outcome, in a population of mechanically ventilated COVID-19 patients transferred to a tertiary ARDS/ECMO referral center.
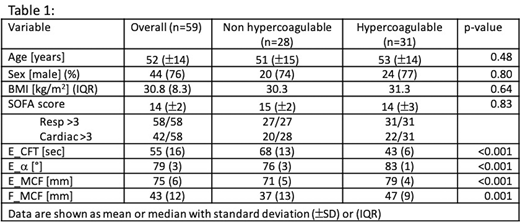
Methods: All COVID-19 patients receiving mechanical ventilation at our center between April 3 and June 15, 2020 were assessed with ROTEM. Testing performed included at least ExTEM and FibTEM. Patients were classified as hypercoagulable (HC) or not (nHC) using the following criteria from ROTEM: ExTEM clot formation time (E_CFT)< 40 sec, alpha (∝) angle >79° and, either ExTEM or FibTEM maximum clot firmness (E_MCF or F_MCF) >70mm or >24mm, respectively. Outcomes, assessed at discharge from our ICU, included thromboembolic events (TE: composite of deep vein thrombosis, pulmonary embolism and ischemic stroke), acute kidney injury (AKI: AKIN stage >2 with or without dialysis), duration of mechanical ventilation, requirement for ECMO, and death. Difference between groups was determined using the chi-square or Fisher-exact test for categorical data and a t-test for continuous variables respectively, using p<0.05 as significant.
Results: Of 59 patients included, 31 were hypercoagulable (HC) on admission. Mean (SD) age was 52 (14), and SOFA score on admission was high 15 (2). The severity of disease was similar in both groups especially for the cardiac and respiratory SOFA components (Table 1). The composite outcome of TE was not different between the groups (HC 9/31, nHC 6/28, p=0.7). The composite renal outcome was not different (HC 18/31 vs nHC 16/28). Mortality rate (29%, HC 9 vs nHC 8), and the duration of ventilation in survivors (HC 22 vs nHC 22 days) were similar in both groups. Requirement for ECMO support was similar (HC 8 vs nHC 12, p= 0.27). Patients were tested with daily viscoelastic tests and, neither fibrinolysis nor DIC were documented. All patients received TE prophylaxis and 34 received therapeutic intravenous heparin for ECMO (n=20) or TE treatment (n=14). Initial ROTEM were conducted on therapeutic heparin in 22 cases (12 HC, 10 nHC).
Conclusion: Our data suggest that in a population of mechanically ventilated patients with severe COVID-19, an early hypercoagulable profile on ROTEM was not associated with an increased risk of thromboembolic events, AKI, prolonged ventilation, ECMO or death during their ICU stay.
Karkouti:Octapharma: Research Funding; Canadian blood services: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal